Recent publications in The Lancet highlight pivotal advancements in dementia research, focusing on risk reduction strategies and comprehensive care approaches. These studies offer valuable insights into modifiable risk factors, prevention methods, and person-centered care techniques, paving the way for improved dementia management and potential risk reduction.
Understanding Dementia Risk Factors
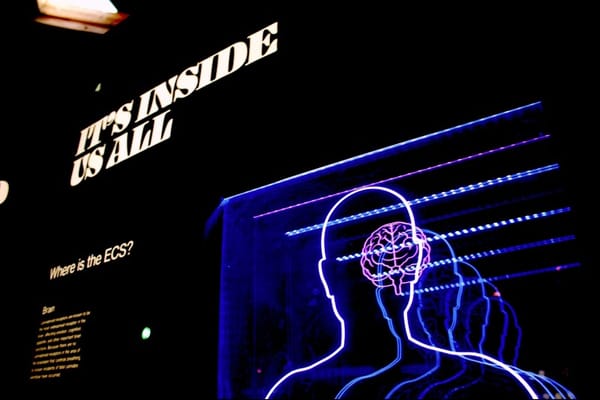
Dementia risk factors can be categorized into modifiable and non-modifiable factors, with recent research highlighting the potential for risk reduction through lifestyle changes and management of certain health conditions. Understanding these risk factors is crucial for developing effective prevention strategies and improving overall brain health.
Non-modifiable risk factors include:
- Age: The risk of dementia increases significantly with advancing age, particularly after 65 1.
- Genetics: Certain genetic mutations can increase the risk of specific types of dementia, such as Alzheimer's disease and Huntington's disease 1.
- Family history: Having a close relative with dementia may increase one's risk, although it's not a guarantee of developing the condition 1.
Modifiable risk factors, which offer opportunities for intervention and risk reduction, include:
- Cardiovascular health: Conditions such as hypertension, high cholesterol, and atherosclerosis are significant risk factors for vascular dementia and may also contribute to Alzheimer's disease 1 2.
- Diabetes: This condition increases the risk of both Alzheimer's disease and vascular dementia 1.
- Smoking: Several studies have found that smoking significantly increases the risk of cognitive decline and dementia 1.
- Alcohol consumption: While moderate drinking may have a protective effect, heavy alcohol use appears to increase dementia risk 1.
- Physical inactivity: Lack of regular exercise is associated with a higher risk of cognitive decline 2.
- Obesity: Excess body fat, particularly in midlife, is linked to an increased risk of dementia 3.
- Education level: Lower educational attainment is associated with a higher risk of dementia 3.
- Hearing loss: Untreated hearing impairment in later life is a significant risk factor 3.
- Social isolation: Limited social interactions in older age can contribute to cognitive decline 3.
- Depression: Late-life depression may be both a risk factor and an early indicator of dementia 4.
- Air pollution: Exposure to air pollutants, particularly from traffic exhaust and wood burning, has been associated with increased dementia risk 4.
Recent research has identified additional risk factors:
- Elevated homocysteine levels: Higher-than-average blood levels of this amino acid are strongly associated with an increased risk of Alzheimer's disease and vascular dementia 1.
- Mild cognitive impairment: Individuals with mild cognitive impairment have a significantly higher risk of developing dementia compared to the general population 1.
- Vision impairment: Untreated vision problems in later life may contribute to cognitive decline 3.
A comprehensive study by the Lancet Commission on dementia prevention, intervention, and care suggests that addressing these modifiable risk factors could potentially prevent or delay up to 45% of dementia cases 3. This underscores the importance of a life-course approach to dementia prevention, addressing risk factors from childhood through late life.
It's important to note that while these risk factors have been associated with increased dementia risk, they do not necessarily cause dementia directly. Some may be early indicators of an impending dementia diagnosis rather than causal factors 3. Nonetheless, managing these risk factors through lifestyle modifications and appropriate medical care can contribute to overall brain health and potentially reduce the risk of cognitive decline.
Ongoing research continues to explore the specific mechanisms by which these risk factors influence dementia risk, aiming to develop more targeted prevention strategies and interventions. As our understanding of dementia risk factors evolves, it offers hope for more effective prevention and management of this complex condition.
Sources:
- (1) Dementia Risk Factors | Stanford Health Care
- (2) Dementia Risk Reduction - CDC
- (3) Tackle these 14 factors to lower dementia risk, report suggests - CNN
- (4) Dementia - Symptoms and causes - Mayo Clinic
Emerging Research in Prevention
Recent research has highlighted several promising avenues for dementia prevention, building on our understanding of modifiable risk factors and potential interventions. The Lancet Commission's 2024 report on dementia prevention, intervention, and care provides compelling new evidence and insights into emerging prevention strategies.
One significant finding is the potential impact of treating vision and hearing loss on dementia risk. The report suggests that addressing untreated vision loss could prevent up to 4% of dementia cases 1. This builds on previous research indicating that hearing loss is a major modifiable risk factor for dementia. Interventions targeting sensory impairments may offer a practical approach to reducing dementia risk in older adults.
Physical activity continues to be a key focus of prevention research. A growing body of evidence supports the cognitive benefits of regular exercise, with studies suggesting that even moderate levels of physical activity can significantly reduce dementia risk 2. The Lancet Commission emphasizes the importance of promoting physical activity across the lifespan, particularly in midlife and older age.
Nutrition and diet are also emerging as important areas of prevention research. While no single "dementia prevention diet" has been identified, studies indicate that Mediterranean-style diets rich in fruits, vegetables, whole grains, and lean proteins may offer protective benefits against cognitive decline 3. Additionally, research is exploring the potential neuroprotective effects of specific nutrients and dietary patterns.
Social engagement and cognitive stimulation are gaining recognition as crucial factors in dementia prevention. The Lancet report highlights the importance of maintaining social connections and engaging in mentally stimulating activities throughout life 1. This aligns with the "cognitive reserve" hypothesis, which suggests that intellectually engaging activities may help build resilience against cognitive decline.
Emerging research is also focusing on the role of sleep in dementia prevention. Studies have linked poor sleep quality and sleep disorders with an increased risk of cognitive decline and dementia 3. Interventions targeting sleep hygiene and treating sleep disorders may offer a new avenue for reducing dementia risk.
The concept of multimodal interventions is gaining traction in prevention research. Rather than focusing on single risk factors, studies are exploring the potential benefits of comprehensive lifestyle interventions that address multiple risk factors simultaneously. For example, the FINGER study (Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability) demonstrated that a multidomain intervention targeting diet, exercise, cognitive training, and vascular risk monitoring could improve or maintain cognitive function in at-risk older adults 2.
Advances in biomarker research are opening up new possibilities for early intervention and prevention. The ability to detect Alzheimer's-related changes in the brain years before symptoms appear may allow for targeted interventions in high-risk individuals 4. Ongoing clinical trials, such as the Anti-Amyloid Treatment in Asymptomatic Alzheimer's (A4) study, are exploring whether early intervention with anti-amyloid therapies can prevent or delay cognitive decline in people at risk of Alzheimer's disease 2.
Genetic research is also contributing to our understanding of dementia risk and prevention. While some genetic risk factors are non-modifiable, studies suggest that lifestyle interventions may be particularly beneficial for individuals with genetic predispositions to dementia 5. This highlights the potential for personalized prevention strategies based on genetic risk profiles.
The role of inflammation in dementia is an active area of research, with studies exploring the potential of anti-inflammatory interventions in prevention. Some researchers are investigating whether existing anti-inflammatory medications might offer protective benefits against cognitive decline 3.
Finally, the emerging field of digital health technologies is opening up new possibilities for dementia prevention. Mobile apps, wearable devices, and online platforms are being developed to support cognitive training, monitor risk factors, and promote healthy lifestyle behaviors 2. These technologies may offer scalable, personalized approaches to dementia prevention in the future.
While these emerging areas of research offer promising directions for dementia prevention, it's important to note that much of this work is still in its early stages. Long-term, large-scale studies are needed to confirm the effectiveness of many of these approaches. Nonetheless, the growing body of evidence supporting the potential for dementia prevention through lifestyle modifications and targeted interventions offers hope for reducing the global burden of dementia in the coming years.
Sources:
- (1) Dementia prevention, intervention, and care 2024 - The Lancet
- (2) Can Alzheimer's Disease Be Prevented?
- (3) Advances in Alzheimer's Disease & Related Dementias Research
- (4) New group training tool for the prevention of dementia - ScienceDaily
- (5) 7 new developments in dementia research in 2019
Advancements in Dementia Care
Recent advancements in dementia care have significantly improved the quality of life for individuals living with dementia and their caregivers. These innovations span various aspects of care, from technological solutions to personalized interventions.
One of the most promising areas of development is in cognitive support technologies. These tools are designed to provide essential assistance to individuals with dementia, helping them maintain independence and improve their daily functioning. For example, interactive technologies customized for people with dementia have emerged as a significant focus within Human-Computer Interaction (HCI) research 1. These technologies aim to address the unique challenges faced by dementia patients in their day-to-day lives.
Artificial Intelligence (AI) and Large Language Models (LLMs) are being integrated into existing dementia care technologies, offering substantial potential for enhancing the well-being of both patients and caregivers 1. AI-powered solutions have shown improvements in patients' daily functioning, quality of life, and overall well-being. They can assist with activities of daily living (ADLs) such as dressing, grooming, and eating, which not only supports the patient but also helps reduce caregiver burnout 2.
Wearable technologies have become increasingly important in dementia care. Devices like Buddi, Telecare, and Careline are specifically designed for dementia patients and incorporate features such as fall detection 3. These wearables use inertia measurement units to monitor the wearer's movements and can alert caregivers or emergency services in case of a fall or other concerning events.
Remote monitoring platforms are another significant advancement in dementia care. These systems allow for the collection of data on the progression of the disease for individual patients, enabling the creation of personalized care profiles. By recognizing changes in patterns compared to a baseline, these platforms can guide the implementation of other technological interventions to align with the patient's specific needs and stage of the disease 3.
Robotics has also made strides in dementia care, particularly in addressing psychological distress. Robotherapy has shown promising results in reducing agitation, depression, anxiety, impulsiveness, restlessness, and chronic pain among dementia patients 4. Commercially available robots like PARO, NeCORO, Ollie the Baby Otter, and Hugby Laugh are being used to provide companionship and emotional support to patients.
Telehealth services have expanded to include specialized programs for dementia care. For instance, the Tele-Savvy program offers online caregiver education and training, teaching caregivers to think like nurses through weekly video conferences, daily video lessons, and interactive learning about other caregivers' experiences 2.
Social media platforms are being leveraged to promote healthy aging in seniors with dementia and to provide support for caregivers. These platforms can increase access to health information and education, potentially relieving some of the burdens on caregivers 2.
Advancements in early detection technologies are also crucial in dementia care. Research is underway to develop non-invasive methods for detecting dementia, such as speech and gait analysis 4. Machine learning models are being developed to detect dementia early based on brain imaging, including MRI and PET scans 4.
Modern memory care communities are raising their standards by implementing person-centered care approaches, creating dementia-friendly environments, and offering specialized training for staff 2. These improvements aim to provide more effective and compassionate care for individuals with dementia.
It's important to note that while these technological advancements offer significant benefits, they also raise concerns about privacy and data security. Ensuring patient privacy is central to the adoption of technology-based dementia care solutions 4. Patients and caregivers must be informed about data collection and usage protocols, and solution providers must prioritize data privacy and security to foster a trusted environment for care delivery.
As research continues and technology evolves, we can expect to see even more innovative solutions in dementia care. The focus remains on providing personalized, effective care that enhances the quality of life for individuals with dementia while supporting caregivers in their crucial role.
Sources:
- (1) Advancements in Technology to Support Dementia Care - arXiv
- (2) Memory Care Technology: Trends and Innovations Shaping the Future
- (3) Care tech: exploring the latest trends in dementia care - CDP
- (4) Technology for dementia care: benefits, opportunities and concerns
Early Detection and Intervention
Early detection and intervention are crucial aspects of managing Alzheimer's disease and other forms of dementia. Recognizing the signs and symptoms early can lead to better outcomes for patients and their families.
One of the most common early signs of Alzheimer's disease is memory loss, particularly forgetting recently learned information. This may manifest as asking the same questions repeatedly or increasingly relying on memory aids or family members for tasks previously handled independently. 1 However, it's important to note that occasional forgetfulness, such as misplacing items and later remembering where they are, is a typical age-related change and not necessarily indicative of dementia. 1
Other early warning signs include:
- Difficulty planning or solving problems, such as trouble following familiar recipes or managing finances 1
- Challenges in completing familiar tasks at home, work, or in leisure activities 1
- Confusion with time or place, including losing track of dates, seasons, or the passage of time 1
- Vision problems that may affect balance, reading, or judging distance and color contrast 1
- Problems with words in speaking or writing, such as difficulty following or joining conversations 1
- Misplacing things and being unable to retrace steps to find them 1
- Decreased or poor judgment, particularly in dealing with money or personal grooming 1
- Withdrawal from work or social activities 1
- Changes in mood and personality, including increased confusion, suspicion, depression, fear, or anxiety 1
Early detection of these signs is essential for several reasons. It allows for timely access to information, care, and support for individuals living with Alzheimer's and other dementias. Many people living with Alzheimer's are not diagnosed, and even among those who are, a large number are unaware of their diagnosis. An early diagnosis can improve the quality of care and quality of life, potentially reducing the financial and emotional impact of the disease. 2
For healthcare providers, several tools and resources are available to help detect and diagnose cognitive impairment as early as possible. These include the KAER (Kickstart, Assess, Evaluate, Refer) Approach, which provides a framework for identifying and assessing individuals at risk for cognitive impairment. 2
Biomarkers are emerging as promising tools for early detection. These biological indicators can potentially detect Alzheimer's before symptoms begin, allowing for earlier intervention. Researchers are studying various biomarkers, including beta-amyloid and tau levels in cerebrospinal fluid, and brain changes detectable through imaging. 3
Neuroimaging techniques, such as structural MRI and functional PET scans, are also valuable tools for early detection. These can reveal brain shrinkage, reduced glucose metabolism, or the presence of amyloid plaques, all of which can be early indicators of Alzheimer's disease. 3
Early diagnosis and intervention can result in substantial benefits for patients, carers, and healthcare systems. It allows time for all concerned to adjust while the patient can still actively engage, and offers access to advice, financial support, and both non-pharmacological and pharmacological treatments. 4
While there are currently no disease-modifying treatments that can reverse the initial pathological changes of Alzheimer's, early diagnosis allows for better management of symptoms and planning for the future. Many patients with mild-to-moderate Alzheimer's dementia can maintain a good quality of life for several years with access to optimal treatments and resources. 4
It's crucial to consult a doctor for a complete assessment if several of these warning signs are present. The diagnostic process typically involves a comprehensive medical assessment, including medical history, physical examination, laboratory tests, cognitive testing, brain imaging, and possibly a psychiatric assessment. 5
Early detection and intervention in Alzheimer's disease and other dementias represent a significant opportunity to improve outcomes and quality of life for patients and their families. As research progresses, we can expect more advanced and accurate methods for early detection, potentially leading to more effective interventions and treatments in the future.
Sources:











Member discussion