Living with HIV presents numerous challenges, and one often overlooked aspect is how the virus and its treatment affect the body's microbiome - the trillions of microorganisms that inhabit our gut and mouth. A groundbreaking study has shed new light on this complex relationship, revealing how different HIV treatments can significantly alter the balance of these vital microbial communities.
Key Takeaways:
- HIV infection reduces microbial diversity in both the gut and mouth.
- Different antiretroviral therapies (ART) have distinct effects on the microbiome.
- Certain beneficial bacteria increase with some treatments, while potentially harmful ones decrease.
- Microbiome changes may be linked to weight gain in some patients on specific HIV medications.
- The study highlights the need for personalized treatment approaches considering microbiome impacts.
The human body is home to trillions of microscopic organisms, collectively known as the microbiome. These tiny inhabitants play crucial roles in our health, from aiding digestion to supporting our immune system. For people living with HIV, maintaining a healthy microbiome can be especially challenging. A new study published in Scientific Reports has uncovered fascinating details about how HIV and its treatments affect the delicate balance of microbes in both the gut and mouth.
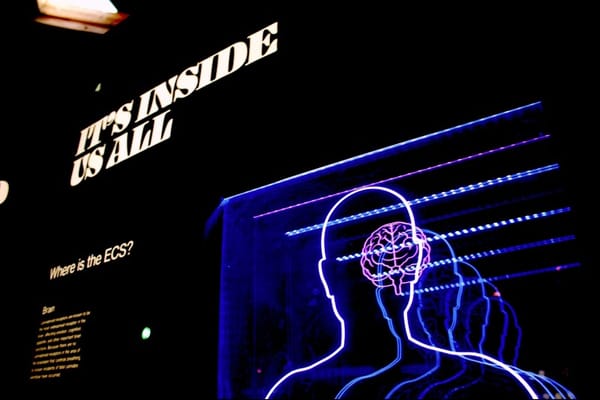
The Microbiome: Your Body's Hidden Ecosystem
Before diving into the study's findings, it's important to understand what the microbiome is and why it matters. Think of your body as a bustling city, with different neighborhoods (organs) populated by diverse communities of microbes. The gut and mouth are two particularly important "neighborhoods" in this microbial metropolis.
In a healthy person, these microbial communities exist in a carefully balanced state. They help break down food, produce essential vitamins, and even communicate with our immune system. When this balance is disrupted - a condition known as dysbiosis - it can lead to various health problems.
HIV's Impact on the Microbiome
The study, conducted by researchers at Karolinska Institutet in Sweden, compared the microbiomes of people living with HIV to those of healthy individuals. They found that HIV infection itself leads to a significant reduction in microbial diversity. This means fewer different types of bacteria are present, which can make the microbiome less resilient and potentially more susceptible to harmful invaders.
Specifically, the researchers observed:
- Lower overall bacterial richness in both the gut and mouth of people with HIV
- An increase in potentially harmful bacteria like Klebsiella and Escherichia-Shigella
- A decrease in beneficial bacteria such as Bifidobacterium and Faecalibacterium
These changes can have far-reaching effects on a person's health, potentially contributing to inflammation, digestive issues, and even affecting how well medications are absorbed.
Not All Treatments Are Created Equal
One of the study's most intriguing findings is that different types of antiretroviral therapy (ART) - the medications used to treat HIV - can have distinct effects on the microbiome. The researchers focused on two main classes of HIV drugs:
- Integrase Strand Transfer Inhibitors (INSTIs)
- Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Here's what they discovered:
INSTI Treatment:
- Increased levels of beneficial bacteria like Bifidobacterium and Faecalibacterium in the gut
- Higher abundance of Veillonella bacteria in the mouth
NNRTI Treatment:
- Enrichment of bacteria like Gordonibacter and Megasphaera in the gut
- Higher levels of Fusobacterium and Alloprevotella in the mouth
These differences are significant because they suggest that the choice of HIV treatment could have broader implications for a patient's overall health beyond just controlling the virus.
The Weight Gain Connection
An unexpected finding of the study was a potential link between certain microbiome changes and weight gain - a side effect reported by some patients on HIV medications, particularly INSTIs. The researchers found that people with higher body mass index (BMI) tended to have more Bifidobacterium and Dorea bacteria in their gut.
While this doesn't prove that these bacteria cause weight gain, it raises interesting questions about the complex relationship between HIV treatment, the microbiome, and metabolism. This could be an important consideration for doctors when choosing the most appropriate treatment for each patient.
Beyond the Gut: The Oral Microbiome
The study also highlighted changes in the mouth's microbial community, an area often overlooked in HIV research. People with HIV showed differences in their oral microbiome compared to healthy individuals, including:
- Higher levels of bacteria associated with gum disease
- Changes in bacteria that help maintain a healthy oral pH balance
These findings underscore the importance of good dental hygiene and regular check-ups for people living with HIV, as they may be at higher risk for oral health problems.
What Does This Mean for Patients?
While this research provides valuable insights, it's important to remember that HIV treatment decisions should always be made in consultation with a healthcare provider. The study's findings don't mean that one type of treatment is universally better than another. Instead, they highlight the need for a personalized approach to HIV care that considers the whole person, including their microbiome.
Some potential implications for patients and healthcare providers include:
- Considering probiotic supplements or dietary changes to support a healthy microbiome
- Monitoring for weight changes and metabolic issues more closely with certain treatments
- Placing greater emphasis on oral health as part of overall HIV care
Looking to the Future
This study opens up exciting new avenues for HIV research and treatment. Future studies might explore:
- Whether targeted probiotic therapies could help restore a healthy microbiome in people with HIV
- If microbiome testing could help predict which patients are more likely to experience certain side effects from treatment
- The development of new HIV medications that have less impact on the microbiome
Conclusion
The complex interplay between HIV, its treatments, and the human microbiome is a fascinating area of research with real-world implications for patient care. As our understanding of this relationship grows, it may lead to more personalized and effective approaches to managing HIV and improving overall health for those living with the virus.
While the science can be complex, the takeaway for patients is clear: your microbiome matters. Talking to your doctor about how your HIV treatment might affect these invisible but important communities of microbes could be an important step in taking control of your health.
Remember, HIV treatment has come a long way, and with proper care, people living with HIV can lead long, healthy lives. This research is just one more tool in the ongoing effort to improve that care and ensure the best possible outcomes for every patient.











Member discussion