The intricate relationship between gut microbiota, metabolic health, and Alzheimer's disease (AD) has become a focal point of cutting-edge research. A recent review published in Experimental & Molecular Medicine sheds light on how gut microbiota-derived metabolites may influence mitochondrial and endolysosomal dysfunction in AD, particularly in the context of metabolic syndrome. This comprehensive article explores the key findings and implications of this groundbreaking research.
The Gut-Brain Axis: A New Frontier in Alzheimer's Research
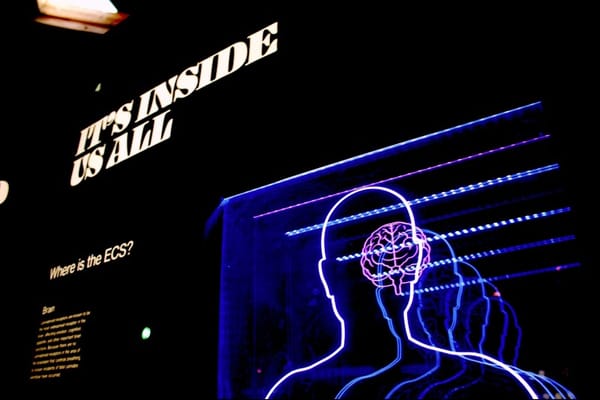
The gut-brain axis has emerged as a crucial area of study in understanding the development and progression of Alzheimer's disease. Recent evidence suggests that changes in gut microbiota composition and their metabolites may play a significant role in AD pathology. This connection becomes even more intriguing when considering the link between metabolic disorders and AD risk.
Metabolic syndrome, characterized by conditions such as obesity, diabetes, and hypertension, has been strongly associated with an increased risk of developing AD. The common thread between these seemingly disparate conditions may lie in the dysfunction of two critical cellular components: mitochondria and the endolysosomal network (ELN).
Mitochondrial Dysfunction: The Energy Crisis in Alzheimer's
Mitochondria, often referred to as the powerhouses of the cell, play a crucial role in energy production and cellular homeostasis. In the context of AD and metabolic syndrome, mitochondrial dysfunction has been identified as a key contributor to disease progression.
Research has shown that mitochondrial abnormalities are prevalent in the brains of AD patients. These dysfunctions can manifest in various ways:
- Impaired energy metabolism
- Disrupted mitochondrial dynamics (fusion and fission)
- Compromised mitophagy (the process of removing damaged mitochondria)
- Altered interactions between mitochondria and the endoplasmic reticulum
- Dysregulation of the mitochondrial antioxidant system
These mitochondrial impairments not only contribute to the energy crisis observed in AD but also exacerbate the accumulation of toxic proteins like amyloid-beta (Aβ) and tau, hallmarks of the disease.
Endolysosomal Network: The Cellular Recycling System Gone Awry
The endolysosomal network, comprising various intracellular membranous organelles, is essential for cellular waste management and protein trafficking. In AD and metabolic disorders, dysfunction of the ELN can lead to:
- Abnormal processing of amyloid precursor protein (APP)
- Impaired degradation of Aβ and hyperphosphorylated tau
- Disrupted cellular signaling and metabolism
Recent genetic analyses have highlighted the importance of autophagic and endolysosomal genes in late-onset AD risk, underscoring the critical role of ELN function in disease pathogenesis.
The Microbiota Connection: How Gut Metabolites Influence Brain Health
The gut microbiota produces a vast array of metabolites that can influence host physiology, including brain function. In the context of AD and metabolic syndrome, several key metabolite classes have emerged as potential regulators of mitochondrial and endolysosomal function:
Amino Acid Metabolites
Tryptophan derivatives, such as indole-3-propionic acid (IPA), have shown neuroprotective properties by reducing oxidative stress and inflammation. Kynurenine pathway metabolites, on the other hand, can have both neuroprotective and neurotoxic effects depending on the specific compound.
Fatty Acid Metabolites
Short-chain fatty acids (SCFAs), particularly butyrate, have demonstrated potential in improving mitochondrial function and reducing neuroinflammation. These metabolites can influence gene expression through histone deacetylase (HDAC) inhibition, potentially attenuating AD progression.
Bile Acids
Secondary bile acids, produced by gut bacteria from primary bile acids, can affect glucose and lipid metabolism. Some bile acids, like tauroursodeoxycholic acid (TUDCA), have shown promise in inhibiting Aβ accumulation and improving mitochondrial function.
Other Metabolites
Gamma-aminobutyric acid (GABA) and lactate, both produced by certain gut bacteria, may influence AD pathogenesis through modulation of neuroinflammation and energy metabolism.
Therapeutic Implications: Targeting the Gut-Brain Axis
Understanding the role of gut microbiota-derived metabolites in AD and metabolic syndrome opens up new avenues for therapeutic interventions. Potential strategies include:
- Probiotic supplementation to modulate gut microbiota composition
- Prebiotic interventions to support beneficial bacteria growth
- Targeted metabolite supplementation (e.g., SCFAs or specific amino acid derivatives)
- Dietary interventions to promote a healthy gut microbiome
These approaches aim to restore balance to the gut microbiota, potentially mitigating the detrimental effects of metabolic syndrome on mitochondrial and endolysosomal function in AD.
Future Directions: Unraveling the Complexity
While the research presented in this review offers exciting insights into the gut-brain axis in AD and metabolic syndrome, many questions remain unanswered. Future studies should focus on:
- Elucidating the specific mechanisms by which gut metabolites influence mitochondrial and endolysosomal function
- Identifying key bacterial species and metabolites that play protective or detrimental roles in AD pathogenesis
- Developing targeted interventions to modulate the gut microbiome for AD prevention and treatment
- Investigating the potential synergistic effects of combining gut-targeted therapies with traditional AD treatments
Conclusion: A Holistic Approach to Alzheimer's Prevention and Treatment
The emerging understanding of the gut microbiota's role in AD and metabolic syndrome highlights the need for a more holistic approach to disease prevention and treatment. By considering the intricate connections between gut health, metabolism, and brain function, researchers and clinicians may be able to develop more effective strategies to combat Alzheimer's disease and related metabolic disorders.
As we continue to unravel the complex relationships between gut microbiota, metabolites, and cellular dysfunction in AD, we move closer to a future where personalized, microbiome-based interventions could play a crucial role in maintaining cognitive health and preventing neurodegenerative diseases.
Citations:











Member discussion