A recent study led by researchers from the University of Cambridge and the Helmholtz Munich Institute of Neurogenomics has uncovered over 140 new genetic risk loci associated with restless leg syndrome (RLS), significantly advancing our understanding of this common yet poorly understood condition. Published in Nature Genetics, the findings could pave the way for new treatment options and improve the quality of life for millions affected by RLS worldwide.
The Role of Glutamate Receptors in RLS
Research has identified that increased glutamatergic activity, particularly in the thalamus, plays a significant role in restless leg syndrome (RLS). Elevated levels of glutamate and glutamine in the thalamus have been correlated with increased wakefulness during sleep periods, suggesting that glutamate may contribute to the arousal disturbances seen in RLS patients[2][4]. This glutamatergic hyperactivity contrasts with the dopaminergic system, which is more closely associated with periodic leg movements during sleep[2]. The identification of glutamate receptors 1 and 4 as genetic risk loci further supports the involvement of glutamatergic pathways in RLS, offering potential targets for therapeutic intervention[1]. Balancing glutamate and GABA activity could be crucial for managing RLS symptoms, as medications that enhance GABA activity have shown efficacy in reducing symptoms[3][5].
Mendelian Randomisation and RLS
Mendelian randomisation has revealed that restless leg syndrome (RLS) is a causal risk factor for type 2 diabetes, highlighting the interconnected nature of these conditions[2][3][5]. This technique uses genetic variants as instrumental variables to assess the causal relationships between traits, providing robust evidence that RLS can increase the likelihood of developing diabetes[1][2]. These findings underscore the importance of considering comorbid conditions in the management and treatment of RLS, as addressing one condition may have beneficial effects on the other[1][5].
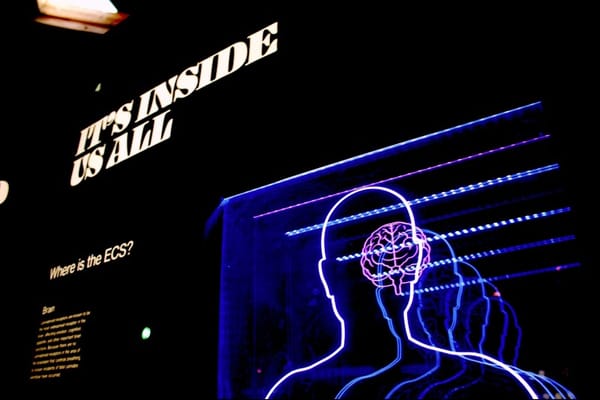
Implications of Neurogenesis in RLS
Recent studies have highlighted the role of neurogenesis in the pathogenesis of restless leg syndrome (RLS), suggesting that the condition may be rooted in neurodevelopmental processes. Genetic variants linked to RLS have been associated with the growth and development of nerve cells, indicating that disruptions in neurogenesis and neuronal circuit formation could underlie the disorder[2][4]. This perspective is supported by findings that implicate genes involved in neurogenesis, such as *MEIS1* and *MEIS2*, which are crucial for the development of the striatum and other brain regions relevant to RLS[2]. These insights not only enhance our understanding of RLS as a neurodevelopmental disorder but also open new avenues for therapeutic strategies targeting neurogenesis pathways[1][4].
Genetic Variants and RLS
Genetic studies have identified several variants associated with restless leg syndrome (RLS), emphasizing the condition's complex genetic architecture. Genome-wide association studies (GWAS) have pinpointed over 160 genetic risk loci, including significant variants in genes such as *PTPRD*, *BTBD9*, and *MEIS1*[1][2]. These loci contribute to the understanding of RLS's heritability and its potential genetic underpinnings. Notably, variants in glutamate receptor genes, which are crucial for nerve and brain function, have been linked to RLS, suggesting that existing drugs targeting these receptors could be repurposed for treatment[1]. Despite these advances, the exact causative genes remain elusive, and further research is needed to fully elucidate the genetic mechanisms driving RLS[2][3].











Member discussion