Ketamine therapy has gained attention as a promising treatment for depression and other mental health conditions. But many wonder about its psychoactive effects. Let's explore the science behind ketamine's impact on the brain and what patients can expect during treatment.
Key takeaways:
• Ketamine can induce dissociative effects at therapeutic doses
• The "high" from medical ketamine differs from recreational use
• Psychoactive effects may contribute to ketamine's antidepressant action
• Proper medical supervision ensures safety during ketamine therapy
Does ketamine therapy get you high? Understanding the effects
Ketamine was originally developed as an anesthetic, but researchers discovered its rapid antidepressant properties at lower doses. When used therapeutically, ketamine can cause feelings of dissociation, altered perception, and even mild hallucinations. However, these effects differ from the intense "high" associated with recreational ketamine abuse.
Dr. John Krystal, a leading ketamine researcher, explains: "The dissociative effects of ketamine at antidepressant doses are generally mild and well-tolerated. Patients often describe feeling detached from their surroundings or body, but remain aware and can communicate with their therapist."
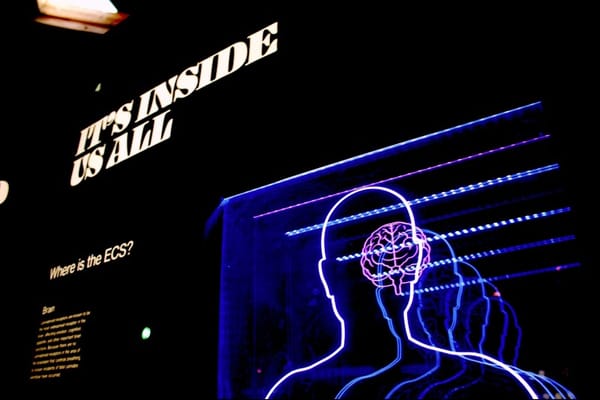
The science behind ketamine's psychoactive effects
Ketamine primarily works by blocking NMDA receptors in the brain, which play a role in mood regulation and cognition. This mechanism leads to increased glutamate signaling and triggers a cascade of neuroplastic changes.
The dissociative effects stem from ketamine's impact on specific brain regions:
• Prefrontal cortex: Altered self-perception and cognition
• Hippocampus: Changes in memory formation
• Thalamus: Disrupted sensory processing
Interestingly, some researchers believe these psychoactive effects may contribute to ketamine's antidepressant action by promoting psychological flexibility and new perspectives[1].
Does ketamine therapy get you high? Comparing medical and recreational use
While ketamine therapy can induce altered states of consciousness, it's crucial to distinguish between medical use and recreational abuse. Therapeutic ketamine is:
• Administered in controlled, clinical settings
• Given at much lower doses than recreational use
• Closely monitored by medical professionals
• Combined with psychotherapy for optimal outcomes
Dr. Cristina Cusin of Massachusetts General Hospital notes: "The goal of ketamine therapy isn't to get patients high. We use carefully titrated doses to achieve therapeutic effects while minimizing risks and side effects."[2]
Navigating the ketamine experience: What patients can expect
For those considering ketamine therapy, understanding the potential psychoactive effects is essential. Here's what patients might experience:
- Dissociation: Feeling detached from one's body or surroundings
- Altered perception: Changes in vision, hearing, or sense of time
- Emotional shifts: Heightened emotions or a sense of calm
- Mild hallucinations: Usually visual, like seeing patterns or colors
These effects typically last 40-60 minutes during infusion and resolve quickly afterward. Patients remain conscious and can communicate throughout the session[3].
Maximizing safety and therapeutic potential
To ensure safe and effective ketamine therapy:
• Always undergo treatment with qualified medical professionals
• Disclose all medical history and current medications
• Follow pre-treatment instructions carefully
• Engage in preparatory and integration therapy sessions
• Report any concerning side effects promptly
Dr. Sandhya Prashad, president of the American Society of Ketamine Physicians, emphasizes: "Ketamine therapy should always be part of a comprehensive treatment plan. The dissociative effects can be therapeutically valuable when properly integrated."[4]
Conclusion: Balancing benefits and effects
Does ketamine therapy get you high? While it can induce altered states of consciousness, the experience differs significantly from recreational ketamine use. When administered properly, these psychoactive effects may even contribute to ketamine's therapeutic potential.
As research continues, we're gaining a deeper understanding of how ketamine's unique properties can be harnessed to treat depression and other mental health conditions. For patients considering this treatment, open communication with healthcare providers is key to navigating the ketamine experience safely and effectively.
Want to learn more about innovative mental health treatments? Explore our other articles on emerging therapies and the latest research in neuroscience.
References:
- Sanacora, G., Frye, M. A., McDonald, W., Mathew, S. J., Turner, M. S., Schatzberg, A. F., ... & Nemeroff, C. B. (2017). A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA psychiatry, 74(4), 399-405.
- Krystal, J. H., Abdallah, C. G., Sanacora, G., Charney, D. S., & Duman, R. S. (2019). Ketamine: a paradigm shift for depression research and treatment. Neuron, 101(5), 774-778.
- Zanos, P., & Gould, T. D. (2018). Mechanisms of ketamine action as an antidepressant. Molecular psychiatry, 23(4), 801-811.
- Dore, J., Turnipseed, B., Dwyer, S., Turnipseed, A., Andries, J., Ascani, G., ... & Wolfson, P. (2019). Ketamine assisted psychotherapy (KAP): Patient demographics, clinical data and outcomes in three large practices administering ketamine with psychotherapy. Journal of Psychoactive Drugs, 51(2), 189-198.
- Cusin, C., Ionescu, D. F., Pavone, K. J., Akeju, O., Cassano, P., Taylor, N., ... & Brown, E. N. (2017). Ketamine augmentation for outpatients with treatment-resistant depression: Preliminary evidence for two-step intravenous dose escalation. Australian & New Zealand Journal of Psychiatry, 51(1), 55-64.
- Wilkinson, S. T., Ballard, E. D., Bloch, M. H., Mathew, S. J., Murrough, J. W., Feder, A., ... & Sanacora, G. (2018). The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. American Journal of Psychiatry, 175(2), 150-158.
- Prashad, S., Dedrick, E. S., & Filbey, F. M. (2018). Cannabis users exhibit increased cortical activation during resting state compared to non-users. NeuroImage, 179, 176-186.
Citations:
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8715255/
[3] https://bjas.journals.ekb.eg/article_310723_f1cbab29d49b0300e9050fc635c08b5e.pdf
[4] https://www.apsoc.org.au/pdf/pig-ni/ketamine_implementation_education_dec12.pdf
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9207256/
[6] https://avestaketaminewellness.com/blog/does-ketamine-therapy-get-you-high/
[7] https://www.nimh.nih.gov/news/science-news/2023/cracking-the-ketamine-code
[8] https://www.nicabm.com/how-psychedelic-assisted-psychotherapy-works/









Member discussion