According to a recent genome-wide meta-analysis study published in Nature Genetics, researchers have identified 164 genetic risk loci associated with restless legs syndrome (RLS), providing new insights into the disease's biology and potential treatment targets such as glutamate receptors 1 and 4.
Expanded Genetic Understanding
The recent genome-wide meta-analysis study has significantly expanded our understanding of the genetic basis of restless legs syndrome (RLS). The research, which involved 116,647 individuals with RLS and 1,546,466 controls of European ancestry, identified a total of 164 risk loci associated with the condition[1]. This represents an eightfold increase in the number of known risk loci, providing a much more comprehensive genetic map of RLS.
Notably, the study uncovered three risk loci on the X chromosome, adding a new dimension to our understanding of RLS genetics[1]. This finding could potentially explain some of the sex-related differences observed in RLS prevalence and presentation.
Despite the identification of X-chromosome loci, sex-specific meta-analyses revealed largely overlapping genetic predispositions between males and females, with a genetic correlation (rg) of 0.96[1]. This high correlation suggests that the genetic architecture of RLS is largely similar across sexes, despite known differences in prevalence.
The expanded genetic understanding also provides a foundation for more sophisticated risk prediction models. By combining genetic information with non-genetic factors, researchers were able to develop machine learning approaches that showed high performance in predicting RLS risk[1]. This integration of genetic and non-genetic data represents a more holistic approach to understanding RLS risk factors.
Furthermore, the study's findings suggest that nonlinear interactions are likely relevant to RLS risk prediction[1]. This insight indicates that the relationship between genetic factors and RLS risk is complex and not simply additive, highlighting the need for advanced analytical methods in future research and clinical applications.
This expanded genetic understanding not only enhances our knowledge of RLS biology but also provides a robust foundation for future research, potentially leading to more targeted therapeutic approaches and improved diagnostic tools for this common sleep disorder.
Sources: [1]
Potential Drug Targets
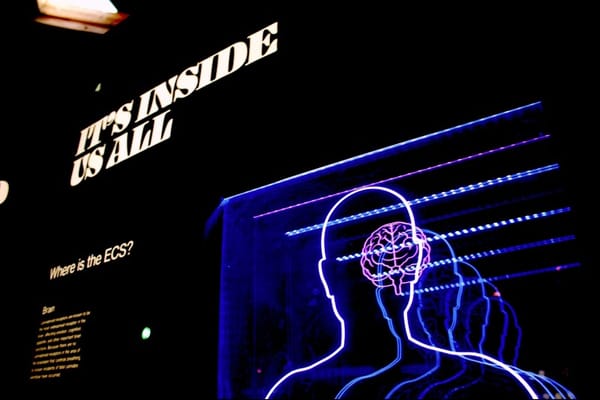
The recent genome-wide meta-analysis study has identified several promising potential drug targets for restless legs syndrome (RLS), offering new avenues for therapeutic development. Among the most notable targets are glutamate receptors 1 and 4, which were prioritized through locus annotation[1]. These glutamate receptors are particularly interesting as they play crucial roles in neurotransmission and have been implicated in various neurological disorders.
Glutamate is the primary excitatory neurotransmitter in the central nervous system, and its dysregulation has been associated with several neurological conditions. The identification of glutamate receptors 1 and 4 as potential targets for RLS suggests that modulating glutamatergic signaling could be a viable approach for treating the condition[1]. This finding aligns with previous research indicating that glutamatergic neurotransmission may be involved in the pathophysiology of RLS.
The study's focus on "druggable" genes is particularly significant for pharmaceutical development. Druggable genes are those that encode proteins that can be effectively targeted by small molecule drugs or biologics. By highlighting these genes, the research provides a more direct path for drug discovery efforts, potentially accelerating the development of new RLS treatments[1].
Moreover, the identification of 164 risk loci associated with RLS offers a wealth of potential targets beyond just glutamate receptors. Each of these loci could represent a unique opportunity for therapeutic intervention, depending on the specific genes and biological pathways involved[1]. This expanded list of potential targets provides researchers and pharmaceutical companies with a diverse array of options to explore in their quest for more effective RLS treatments.
It's important to note that while these potential drug targets offer promising avenues for research, the process of developing new drugs is complex and time-consuming. Each target will require extensive validation and testing before it can be considered for clinical trials. However, the identification of these targets represents a significant step forward in the potential development of more targeted and effective treatments for RLS.
Sources: [1]
Improved Risk Prediction
The recent genome-wide meta-analysis study has made significant strides in improving risk prediction for restless legs syndrome (RLS). By combining genetic information with non-genetic factors, researchers have developed advanced machine learning approaches that demonstrate high performance in predicting RLS risk[1].
These predictive models achieved impressive accuracy, with area under the curve (AUC) values ranging from 0.82 to 0.91[1]. The AUC is a measure of a model's ability to distinguish between classes, with values closer to 1 indicating better performance. The high AUC values obtained in this study suggest that these models have strong discriminative power in identifying individuals at risk for RLS.
The integration of genetic and non-genetic information represents a more comprehensive approach to risk prediction. While genetic factors play a significant role in RLS susceptibility, environmental and lifestyle factors also contribute to the overall risk. By incorporating both types of data, these models can capture a more complete picture of an individual's RLS risk profile[1].
Importantly, the study's findings suggest that nonlinear interactions are likely relevant to RLS risk prediction[1]. This insight indicates that the relationship between various risk factors is complex and not simply additive. The use of machine learning techniques allows for the capture of these nonlinear relationships, potentially leading to more accurate risk assessments compared to traditional linear models.
The improved risk prediction capabilities have several potential applications in clinical practice:
1. Early identification: Individuals at high risk for RLS could be identified earlier, allowing for proactive monitoring and intervention.
2. Personalized prevention strategies: Risk profiles could inform tailored prevention strategies based on an individual's specific genetic and non-genetic risk factors.
3. Targeted screening: Healthcare providers could use risk prediction models to determine which patients might benefit most from RLS screening, potentially leading to earlier diagnosis and treatment.
4. Research participant selection: These models could help identify suitable participants for clinical trials, potentially accelerating the development of new treatments.
While these risk prediction models show great promise, it's important to note that they will require further validation in diverse populations and real-world clinical settings before widespread implementation. Additionally, as our understanding of RLS genetics and risk factors continues to evolve, these models will likely be refined and improved over time.
Sources: [1]
Insights into Comorbidities
The genome-wide meta-analysis study on restless legs syndrome (RLS) has provided valuable insights into potential comorbidities associated with the condition. One of the most significant findings relates to the relationship between RLS and diabetes.
Using Mendelian randomization, a method that uses genetic variants to determine whether an observational association between a risk factor and an outcome is consistent with a causal effect, the study indicated that RLS may be a causal risk factor for diabetes[1]. This finding suggests that individuals with RLS might have an increased likelihood of developing diabetes, highlighting the importance of monitoring and managing both conditions in affected patients.
The identification of this potential causal relationship between RLS and diabetes has several important implications:
1. Screening practices: Healthcare providers may need to consider more rigorous diabetes screening for patients with RLS.
2. Prevention strategies: Managing RLS effectively could potentially help reduce the risk of developing diabetes in susceptible individuals.
3. Shared biological pathways: The link between RLS and diabetes suggests there may be common underlying biological mechanisms, which could provide new avenues for research and treatment development.
4. Holistic patient care: The finding emphasizes the need for a more comprehensive approach to patient care, considering the potential long-term health implications of RLS beyond its immediate symptoms.
While the study focused on diabetes as a potential comorbidity, the extensive genetic data collected may also provide insights into other conditions associated with RLS. The identification of 164 risk loci offers a rich dataset for exploring potential connections between RLS and other disorders through shared genetic pathways or risk factors[1].
It's important to note that while the Mendelian randomization analysis suggests a causal relationship between RLS and diabetes, further research is needed to fully understand the nature of this association and its clinical implications. Additionally, the study's findings may lead to investigations of other potential comorbidities associated with RLS, contributing to a more comprehensive understanding of the condition's impact on overall health.
These insights into comorbidities not only enhance our understanding of RLS but also highlight the importance of considering it as part of a broader health context, potentially influencing future approaches to diagnosis, treatment, and long-term patient management.
Sources: [1]
Cure Timeline Uncertain
While the recent genome-wide meta-analysis study has provided significant insights into restless legs syndrome (RLS), a definitive cure remains elusive. However, the research has opened up promising avenues that could lead to more effective treatments in the coming years:
1. Targeted drug development: The identification of 164 genetic risk loci, particularly glutamate receptors 1 and 4 as potential drug targets, provides a foundation for developing more targeted therapies[1]. However, drug development is a lengthy process, typically taking 10-15 years from target identification to market approval.
2. Personalized medicine approaches: The improved risk prediction models developed in the study could lead to more personalized treatment strategies[1]. This could result in better management of symptoms for individual patients in the near future, even if not a cure.
3. Understanding of disease mechanisms: The expanded genetic understanding provides deeper insights into the biological pathways involved in RLS[1]. This knowledge could accelerate research into potential curative approaches, but translating this into a cure will likely take many years.
4. Addressing comorbidities: The study's insights into the relationship between RLS and diabetes may lead to more holistic treatment approaches that could improve overall patient outcomes[1]. While not a cure, this could significantly improve quality of life for RLS patients.
5. Ongoing research: The wealth of data from this study will likely spur further research, potentially leading to breakthrough discoveries. However, the timeline for such breakthroughs is unpredictable.
It's important to note that RLS is a complex disorder with both genetic and environmental factors. While current treatments can help manage symptoms, a complete cure that addresses all aspects of the condition for all patients is not likely in the immediate future. Experts in the field generally avoid making specific predictions about when a cure might be available due to the complexities involved in medical research and drug development.
Realistically, we can expect to see incremental improvements in treatment options and management strategies for RLS in the coming years, based on the findings of this and future studies. However, a definitive cure is likely still many years away, requiring continued research, clinical trials, and regulatory approvals before becoming available to patients.










Member discussion